Bleeding Gums
30 June, 2025
News
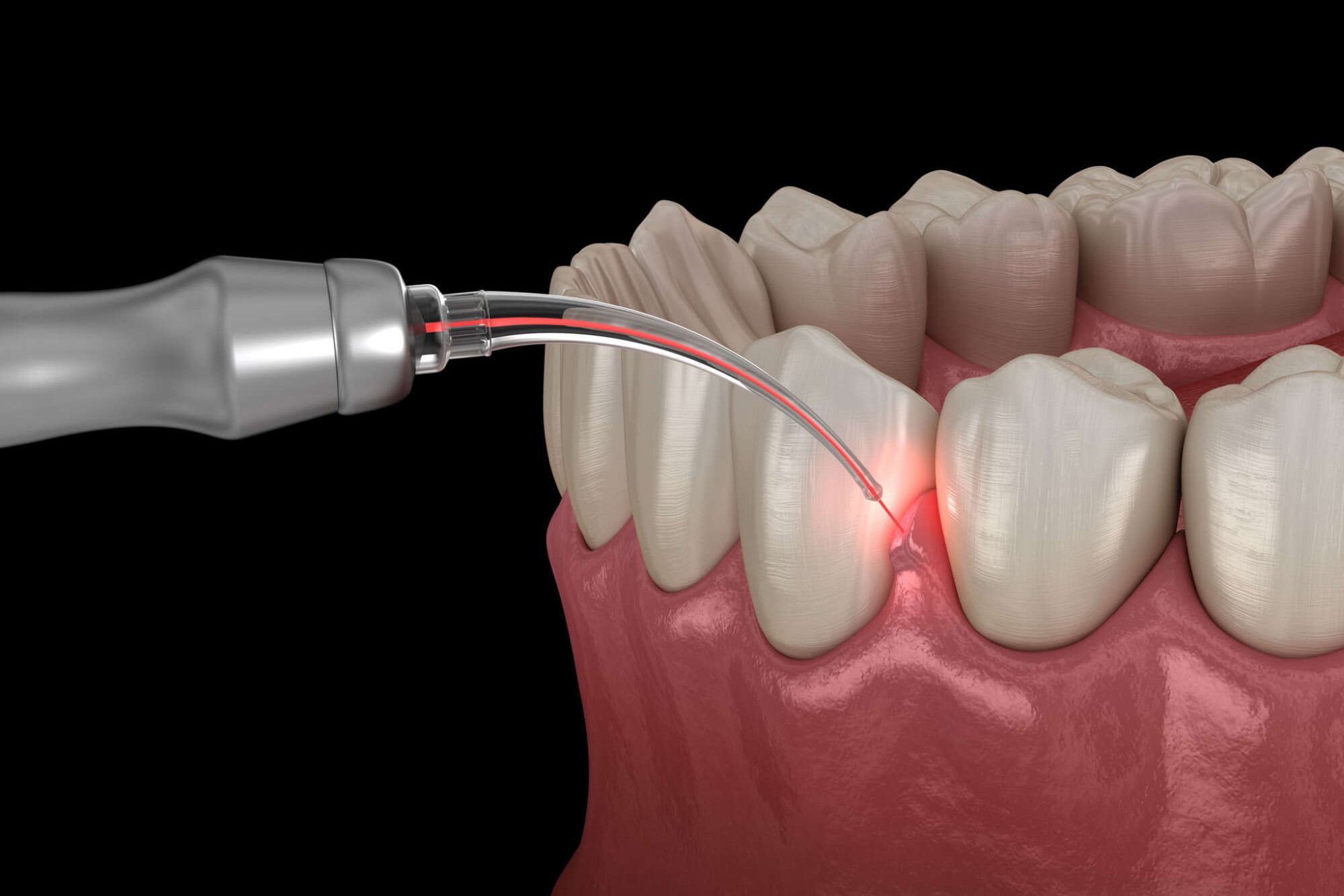
Bleeding Gums

It’s important to address bleeding gums as they can be an early sign of gum disease. Here are some steps you can take:
If bleeding gums persist despite improved oral hygiene practices or if you have other concerns, it’s important to seek professional dental care.
Schedule an appointment with us today!
Dr. Rivas and his team can evaluate your specific situation, diagnose the underlying cause of your bleeding gums, and recommend appropriate treatment options to restore gum health.